Starting in 1996, when the first treatment scheme to stop HIV was created, people began to talk about this infection as something manageable, which had become a chronic disease “like diabetes”.
The latter is a disease characterized by the body’s inability to produce insulin, which processes sugars, and is one of the most common chronic conditions. According to data from the Pan American Health Organization (PAHO), there are some 62 million people with diabetes in the Americas, compared to 2.6 million people living with HIV in the region.
By chance, it is very likely that a person with HIV also deals with diabetes, but perhaps the comparison between how “manageable” one condition can be and another is not as simple as it seems.
The diabetes challenge
In many cases and for many people (including health personnel), HIV infection has become an easier health condition to manage than diabetes, according to the TheBody.com website, which specializes in HIV issues.
Although the science of diabetes drugs has come a long way in recent years, the disease, in general, remains very difficult to manage, as it does not respond only to drugs, but requires lifestyle changes.
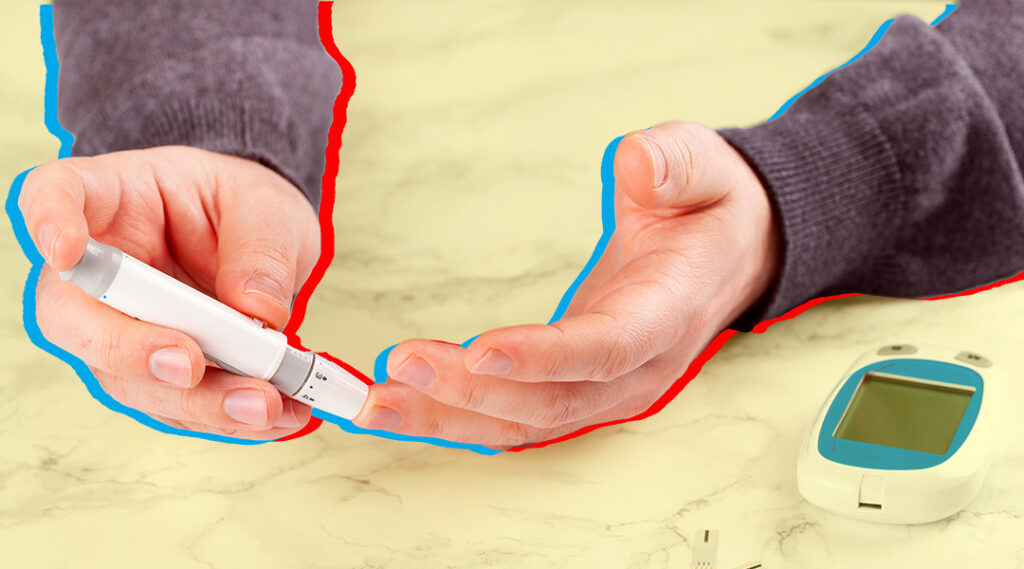
Today, HIV can be treated with just a pill a day, or even injections every month or two, but diabetes necessarily involves a change in habits. “People need to learn to make healthier food choices, reduce or eliminate their alcohol intake, and exercise,” Dr. Mark Watkins told the website. In addition, they must test their blood sugar two to four times a day and take multiple medications, making treatment more complex.
Personal stories
Living with diabetes and living with HIV have different implications for people. The aforementioned website requested, through social networks, testimonials from those who wanted to share their experiences.
Diagnosed with HIV in 1990 and diabetes in 2000, Michael, a 61-year-old San Diego resident, believes diabetes is “far more difficult to cope with right now.” He remembers that HIV was a challenge before the first available drugs, but after he began his treatment in 1996, he was able to resume his job and activities. “HIV has just been a matter of blood tests and the occasional change in medication.”
On the other hand, diabetes has been “a constant battle,” he says. He says he has been on many medications for years, and that his blood sugar is sometimes fine, but then, for no apparent reason, he “goes crazy,” leading to a change of medication and the use of insulin, in addition to constant supervision of diet and exercise.
Added to this, he must prick himself daily to measure his blood sugar levels and his glucose meter sends this data directly to his doctor, which he considers “quite more invasive” than anything to do with HIV.
Constant effort
William, 57, who lives in Philadelphia, was diagnosed with HIV in 1997 and says treatment for the infection didn’t mean much to him. In contrast, complications from his diabetes led him to undergo multiple operations trying to save one of his feet, which ended up being amputated.
He says that seven years ago he underwent a gastric bypass operation, which is used to reduce weight, and managed to lose about 181 kilos to 69, which led to his diabetes remission. Before that, he recalls, “living with the complications of diabetes was physically, emotionally and mentally depressing.”
Medical specialists recognize that curbing diabetes involves learning new habits and that a person’s life cannot be completely changed overnight. You have to take small steps, one at a time.
Giving up sugary drinks, for example, is a step that, on its own, can make a big difference. Walking more or taking the stairs instead of the elevator are other daily decisions that can start to contribute to your health.
And if you’re living with HIV, you most likely have access to a medical team that includes nutrition counseling, which can help you further make the changes needed to combat diabetes.
Remember that to live well with HIV, medical care is key. If you have not started your antiretroviral treatment or you suspended it and want to resume it, come to AHF Latin America and the Caribbean and we will advise you. Locate our offices in your country here.